Introduction
Since its inception in 2008, Advanced Neural Biosciences (ANB) has collaborated with the Immortalist Society (IS), The American Cryonics Society (ACS), and the Cryonics Institute (CI) to research the effects of ischemia (decreased supply of nutrients, oxygen, and/or blood flow to tissues) on cryoprotection and cryopreservation with an understandable emphasis on the brain.
Most of this research has bolstered the concept and practice of providing rapid stabilization and remote blood washout by professional standby teams. Many cryonicists, however, do not have such standby arrangements and are dependent on either rapid response from local volunteers and family members and/or the assistance of local morticians. Even in the case of individuals signed up with professional standby organizations, often the patient is a long distance away from the professional standby team. This can easily result in significant delays before that team can arrive at the patient's location.
Clinical death can also be unexpected as in the case of a sudden and fatal heart attack or other unexpected catastrophic health event, including trauma. On top of that the exact moment of clinical death is difficult to predict in any individual medical case, whether from illness, trauma, or a combination of the two. This can even include patients with terminal/chronic illnesses that are known to be going to result in an individual having a limited amount of time left before clinical death occurs. All these factors mean that even when cryonicists have professional standby arrangements it is extremely wise to also have a backup plan using the assistance of local volunteers, family members, and morticians.
So which procedures can be used by local members and morticians to help improve outcomes and to subject these protocols to experimental research?
Mortician-Assisted Medication Administration
Discussion about the merits and specifics of medications administration in cryonics is basically as old as the field of cryonics itself. Perspectives have ranged from the advocacy of administration of many medications (sometimes more than 20) to just administering the anti-blood clotting medication heparin. While all of these suggestions were made by individuals deeply interested in and deeply dedicated to cryonics, much of the thinking was extrapolated from medical and scientific literature of non-cryonics situations and not from actual experiments specifically directed towards evaluating conditions similar to those faced in dealing with real cryonics patients. This gap was one of the major reasons for the formation of ANB.
During the period of 2014-2016 ANB collaborated with the Alcor Life Extension Foundation to scientifically scrutinize, to the degree reasonably possible, the administration of many medications and fluids upon the quality of brain cryopreservation after ischemia. Our results were mostly sobering in terms of revealing the lack of efficacy of many suggested medications and approaches but they also turned out to be encouraging for some interventions. When judged by perfusion quality of cryoprotectants and ice formation, sodium citrate and heparin produced significant positive effects on the quality of cryopreservation.
After “pre-mortem” administration of these medications, these benefits could still be reaped up to after at least 120 minutes of circulatory arrest (i.e. “clinical death”) and even 150 minutes if cryoprotectant perfusion was conducted at lower arterial perfusion pressures (< 80 mmHg). The catch, however, is that these medications must be administered within a specific time to have this effect. In our research we found that these positive effects could still be observed if either of these substances were given within 15 minutes after circulatory arrest but could no longer be observed if given later than 30 minutes after arrest. This puts the window of opportunity, then, for even heparin or citrate somewhere between 15 minutes and 30 minutes.
The desired response time for these results is so short that it can be challenging for a professional standby team, let alone local morticians to administer these potent medications before the applicable time period runs out.
One potential exception to this rather stringent time of administration requirement concerns the administration of an antibiotic. In principle, morticians can administer and circulate an antibiotic like gentamicin or minocycline to prevent microbial overgrowth during cold transport of the patient to the cryonics facility. This practice is even more important when long transport times are expected (days instead of hours), or if a patient died of a condition that accelerates decomposition such as sepsis. If a patient is at risk for rapid decomposition during long transport times, the more radical step of freezing the patient and foregoing cryoprotection (a so-called “straight freeze”) is a possibility. Another possibility (which will be discussed in more detail below) is to chemically fix the patient to inhibit microbial activity.
One other potential intervention that is worth mentioning is the administration of a so-called “clot busting” agent such as streptokinase. Unlike heparin (or sodium citrate), which can only help prevent blood clotting, clot busters (technically known as “fibrinolytics”) can break up existing blood clots. Research in our lab supports the practice of adding streptokinase to the washout solution immediately before or just after a period of cold transport. This recommendation is consistent with some mainstream organ preservation research in which flushing the organ with a clot buster improves outcome. Ideally this intervention involves perfusion of a liquid using the patient's circulatory system, so a mortician would only be involved with this procedure if (s)he aims to do a field washout or field cryoprotection for the cryonics organization.
An antacid containing aluminum hydroxide and magnesium hydroxide formerly sold under the brand name of “Maalox”) can also be administered to help neutralize hydrochloric acid in the stomach during circulatory arrest and hypothermia to aid in preventing gastric hemorrhage. It is not clear, however, that this intervention provides additional protection because long (multi-day) transport times on water ice are known to increase cellular and vessel permeability regardless. Unlike the other medications, an antacid requires administration through a gastric tube for delivery into the stomach. In some instances, it may be possible for the patient to orally self-administer an antacid prior to death or possibly to have this done very close to clinical death if the patient is in a situation where medical professionals are taking care of the individual.
To summarize, administration of heparin or sodium citrate by a local team member or mortician can be of benefit to the patient, provided this is done rapidly (again within 15 to no more than 30 minutes after circulatory arrest). A suitable antibiotic (like gentamicin) can be administered to protect a patient against microbial overgrowth during long transport times. Clot busters such as streptokinase can be effective during the initial stages of washout or cryoprotection. Administration of an antacid may be of benefit in a small number of cases, but the potential benefits might be offset by long ground or air transport times on water ice.
It is not routine for funeral homes to have chemicals like heparin, sodium citrate and antibiotics on hand, let alone a more sophisticated (and expensive) substance like streptokinase. This means that, optimally speaking, local members or the cryonics organization must supply funeral homes with these medications (preferably through a cooperating physician) while the patient is still terminally ill to allow for timely administration. In practice this means that intervention can only work for morticians who conduct some sort of standby, and administer these drugs prior to transport to the funeral home (not after arrival).
Even in small towns, where funeral homes may be only a very short distance from a local hospital, nursing home, or hospice facility, the “within fifteen minutes” guideline for heparin or sodium citrate should be kept in mind in terms of administration guidelines and one should not be led into a false sense of security due to the close proximity of a local funeral home. The cryonics organization or funeral home could also, as an alternative, request cooperating nurses/other qualified and cooperating health care professionals to administer heparin, even in cases where the mortician is nearby the medical facility.
Mortician-Assisted Blood Substitution (aka “Washout”)
Replacement of the blood with a so-called “organ preservation solution” is one of the core protocols for professional standby teams. In our initial research we investigated the efficacy of this procedure after various periods of circulatory arrest. Blood substitution with a suitable blood replacement is advantageous because it removes the blood (and its ability to clot) and inflammatory cells from the circulation, provides metabolic support, and can assist in cooling if done quickly after pronouncement of clinical death.
However, not all organ preservation solutions are created equal. For example, we found that replacing the blood with just saline (sodium chloride) worsens cryoprotection outcomes. It is important to note this because it means that removal of the blood with a simple salt solution (like saline or Ringer’s solution) is not enough, to obtain better outcomes. m-RPS-2, the carrier solution of CI’s VM-1 vitrification solution, produced better results. A solution named MHP-2 produced the best results and allowed for ice-free cryopreservation of the brain up to 48 hours of cold ischemia . The MHP-2 solution components and the information below concerning mixing proportions are publicly available (i.e., no patent applies to this solution any longer). MHP-2 may be used by anyone wishing to do. Also, mixed-up MHP-2 solution may be available in some situations for purchase by cryonics organizations who may not already be using it in their routine operations. A well-prepared solution of MHP-2 has good shelf life of months or even years at normal refrigerator temperatures but sterile technique and filtration in preparation is required to prevent the glucose acting as growth medium for bacteria. There are no rare or very costly ingredients in MHP-2, and in principle, medications that are not long-term stable in solution can be added last-minute (i.e. streptokinase).
In principle, morticians should be able to do blood substitution because replacement of the blood of a cadaver with an embalming solution is a routine mortuary procedure and the basic principle is the same in using m-RPS-2 or MHP-2. This does not mean that instructing a mortician to use their skills and equipment to replace the blood with an organ preservation solution is an unambiguously sound recommendation, especially when it would entail recirculation of the perfusate. Recirculation of the perfusate is a useful and common procedure and, to some degree, a practical necessity as it helps to manage/decrease the total amount of perfusate that is needed. That is to say, it basically allows one to prepare a smaller amount of solution to be readily available for the procedure than would otherwise be the case.
Although morticians are very well trained and very professional individuals, morticians do not necessarily need to be overly concerned with issues such as maintaining a certain physiological pressure, eliminating all air and particulate matter, and minimizing cellular damage. These considerations are very important for the practice of cryonics. Perfusion at very high pressures (a good rule of thumb is to aim for lower than 100 mmHg arterial pressure) can damage the vessels of the patient and the introduction of air or debris can compromise perfusion. Since the circulatory system of a cryonics patient will need to be utilized again later for cryoprotection after the initial blood washout is accomplished, any (irreversible) damage caused by improper perfusion by a mortician will compromise the quality of cryopreservation that will be carried out later.
Blood substitution normally requires making an incision and placing a cannula in order to remove the blood and to introduce the organ preservation solution. Some professional cryonics standby teams (like Suspended Animation) employ professional human cardiovascular surgeons who open the chest (i.e. perform the median sternotomy surgical procedure) to cannulate the vessels of the heart. This is typically not a routine procedure for many morticians and the two most common routes for obtaining vascular access in mortuary procedures are to make incisions in the femoral- or carotid vessels. Which vessels to access may depend on the skill-sets and work experience/training of the specific mortician and the quality of the vessels (for example, atherosclerosis in elderly patients could be a factor in determining which vessels may and can be used). One advantage of femoral access in mortician assisted blood substitution is that it does leave the integrity of the neck vessels intact for later cryoprotectant perfusion, and better washout of the brain is possible because these vessels have not been compromised.
Cannulation of the neck vessels in mortuary procedures usually only involves cannulation of the carotids as the point of introduction of solutions (with the jugular veins being used for venous return). This approach can, however, compromise brain perfusion in cryonics patients who do not have an intact Circle of Willis. The lack of a so called “normal” Circle of Willis, surprisingly, is not a rare situation. Another disadvantage of carotid-only perfusion is that it generates backflow of the solution through the vertebral arteries, resulting in lower perfusion pressure of the hindbrain, compared to a situation where all neck vessels, the heart, or the femoral vessels would be utilized.
Another option would be to perform washout only of the brain (i.e. head) by cannulating the neck vessels and clamping vessels that supply the rest of the body with blood. This would entail, however, foregoing the benefits of blood substitution for the rest of the body. There is also the question whether this regional washout can be maintained since the movement of the patient during transport may generate some degree of forward blood flow. Remaining blood will also flow to the head if the cryonics organization uses different vessels for cryoprotection (i.e. the heart or femoral vessels).
The data on the benefits of blood substitution support this practice up to at least 1 hour of normothermic ischemia, especially for patients with long projected transport times (1 to 2 days). How practical this procedure is for a cryonics organization is not a research question and depends on issues such as cost, resources, and logistics. Funeral homes usually do not maintain the kind of solutions that would be indicated for blood substitution. Like medications administration, these solutions would have to be stored at cooperating funeral homes (or readily available at local member homes, etc.) or shipped at times of need. This is a non-trivial challenge for any existing cryonics organizations with a geographically diverse (international) membership. It will also entail communicating specific protocol directions to a mortician and some degree of reasonable assurance/probability that these instructions will be complied with.
One issue that blood substitution does not resolve is the progressive leaking of vessels in a time-and temperature dependent fashion. Even the most advanced organ preservation solutions, at this point in time, cannot prevent these time-dependent changes in the permeability of vessels. Patients will still, exhibit a lot of swelling (i.e. edema) during whole-body perfusion with cryoprotectants, despite the benefits of blood substitution. This is especially a problem whole-body cryopreservation. The most logical solution to this problem is not to ship the patient to a cryonics facility for cryoprotection but perform this procedure immediately after cooldown at the funeral home.
Mortician-Assisted Field Cryoprotection
Field cryoprotection (FCP) concerns the practice of doing cryoprotection at the location of the patient prior to transport to the cryonics facility for long-term storage. The reason why this procedure is named “field cryoprotection” and not “field vitrification” is because after completion of cryoprotectant perfusion the patient is maintained and shipped on dry ice, which is still above the temperature at which the vitrification solution turns into a glass. Holding a patient at dry ice temperature for a few days, or even a few weeks, after cryoprotectant perfusion is not assumed to compromise the fine structure of the brain, but some thought needs to be given to the composition of the vitrification solution (see below). Field cryoprotection (i.e. perfusion of an individual cryonics patient with cryoprotectants done away from the actual cryonics providers facility) is usually practiced by circulating a series of bags (or containers or bottles) of solutions of increasing cryoprotectant concentration between 0 and 5 degrees Celsius at low pressures (between 60 mm Hg and 100 mmHg arterial pressure).
In theory, all surgical procedures and cannulation techniques that are adequate for blood washout can also be used for cryoprotection. There are some specific considerations, however, for cryoprotectant perfusion that need to be considered. Vitrification solutions at their highest concentrations have a significantly higher viscosity than organ preservation solutions. Consequently, a mortician cannot run these solutions at the same flow rate as (s)he is used to for embalming. As the concentration of the cryoprotectant increases, the pressure will increase for a given flow rate. This means that the mortician must adjust the flow rate downward as the concentration of cryoprotectant increases. Without these flow rate adjustments perfusion pressures will become extremely high, which will result in a compromise of perfusion and damaged blood vessels. One basic remedy is not to use a pump but gravity-assisted infusion in which the bags are hung at a certain height, which imposes a limit on pressure increases because in such protocols the pressure is determined by the height of the “drop” of the solution.
The high viscosity of the vitrification solution also compromises venous return in whole-body patients. This phenomenon is especially notable in ischemically compromised patients at the later stages of perfusion when viscosity is at its highest, and is observed as poor venous return and slowing flow rates (for a given pressure). To prevent this issue (and prevent the natural tendency to compensate by increasing pump speed in order to increase venous return!) it is important that the venous cannula has the widest interior (lumen) possible and that there is enough gravity-assisted drop to facilitate good venous return. An ideal protocol uses the widest venous cannula available for a patient (allowing for patient size) and incorporates a significant drop of the line from the mortuary table or ice bath to the floor. Naturally, the venous line should never slope upwards coming from the patient!
Cryoprotectant perfusion is also different from blood substitution (“washout”) in that it requires sampling of the outgoing perfusate, from time to time, to guide perfusion and decision making. This requires that the mortician captures the cryoprotectant effluent and reads it with a (handheld) refractometer (or any kind of device that can read concentrations of a solution such as an osmometer). Taking refractive measurements from the patient is not a typical mortician procedure and (s)he is not likely to have the equipment to do this or even any experience in using such a device. If a funeral director or local member cannot provide such measurements, one could choose a protocol that sets a minimum (and recommended) amount of perfusate volume deemed necessary to reach target concentration as inferred from prior case data. This may not be a perfect fit for the patient at hand but it may provide some assurance that adequate amounts of cryoprotectant are introduced.
After completion of cryoprotection the patient needs to be shipped on dry ice instead of water ice by ground or air in an insulated shipping container. This comes with its own set of challenges since it requires the use (or on-site fabrication) of an insulated box that permits long-term maintenance and transport of the patient without temperature changes. There are two distinct challenges in dry ice shipping. Since dry ice does not melt but expands into a gas without first going through the liquid phase, the patient cannot be shipped in a tightly sealed container since the build-up of pressure from the carbon dioxide gas would create an explosion risk. Another important aspect of dry ice shipping is that the patient first needs to be cooled to dry ice temperature, then the dry ice replenished, before authorizing shipment. Cryonics organizations have learned the hard way that just placing dry ice on a patient (in a poorly insulated container) will lead to depletion of the dry ice during transport and the patient going through a damaging freeze-thaw cycle before arrival at the cryonics facility.
As can be surmised from this description of field cryoprotection, a lot of things must come together (quite literally in the case of equipment and supplies) for a mortician to successfully cryoprotect and transport the patient to a cryonics facility. For this reason, field cryoprotection is usually only authorized for international cases, or cases where knowledgeable people can assist in, or oversee, the procedure. It might be possible for a cryonics organization to equip and educate a funeral home in a specific area to do this procedure but this cannot be an overnight decision and requires a lot of effort, training, and documentation.
Vitrification Solution Composition for Field Cryoprotection
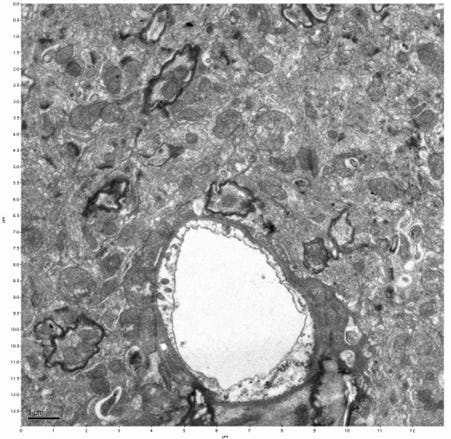
In principle, the same vitrification solution used at the cryonics facility can be used for (mortician-assisted) field cryoprotection. There is one important caveat to this. In cryobiology, vitrification is not an all-or-nothing phenomenon, but rather, depends on cooling rate. That is why vitrification solutions are often reported with a critical cooling rate and critical warming rate necessary to prevent ice formation. The vitrification solutions used by the major cryonics organizations (Alcor’s M22 and CI’s VM-1) fortunately permit very slow cooling rates for vitrification. In field cryoprotection, however, the patient is maintained for days (or even weeks) at dry ice temperature where there is no “rate of cooling” after the patient cools down to that temperature. In such circumstances, ice formation can occur as a function of time. The image below shows two bottles of 60% w/v VM-1 and 65% w/v VM-1 vitrification solution. After only one day of storage at dry ice temperature the 60% w/v solution shows extensive ice formation.
100 ml of 60% w/v VM-1 (left) and 100 ml of 65% w/v VM-1 (right) after 1 day of dry ice temperature storage
This does not necessarily mean that patients perfused to only 60% w/v VM-1 will freeze. Proteins and ions in biological tissues are presumed to facilitate cryoprotection themselves. Our research has shown that brains equilibrated with normal concentrations of VM-1 cryoprotectant do not show ice formation after storage for 2 weeks at dry ice temperature. In ischemically-compromised, or poorly perfused patients, the concentration of cryoprotectant in some areas of the tissue can be sub-optimal, however, and the lack of any kind of “cooling rate” will tip these areas towards freezing in the manner mentioned above. Such frozen areas could further nucleate (i.e., act as a “site” or “nucleus” around which ice crystals can begin to form) other areas where concentrations of cryoprotectant chemicals are low, setting off a “freezing cascade” of poorly protected or unprotected tissue. For this reason, we recommend perfusing to a higher concentration of VM-1 in the case of field cryoprotection. Since standard CI protocol, for example, is to use a 70% w/v solution to reach a 60% w/v target concentration, this is practically possible. Our experiments in isolated hippocampal brain slices show that exposure to 65% w/v VM-1 instead of 60% VM-1 is safe and produces a slight drop in cellular viability but this slight decrease is well worth the risk of producing ice formation.
Mortician-Assisted Aldehyde-Stabilization
One novel procedure that a mortician can perform to improve the outcome of a cryonics case is to stabilize the patient with a chemical fixative prior to transport to the cryonics facility for cryoprotection. Unlike the administration of medications, blood substitution, or cryoprotection, this procedure would be more in the comfort zone of a typical mortician because embalming typically involves the perfusion of a chemical fixative of some kind.
The procedure is called “aldehyde-stabilized cryopreservation” (ASC) and was pioneered by Robert McIntyre at 21st Century Medicine as a superior means to preserve the ultrastructure of the brain. ASC entails perfusion with a chemical fixative prior to cryoprotection. This idea was anticipated by Eric Drexler in his seminal 1986 book “Engines of Creation.” Historically, combining chemical fixation and cryopreservation was not favored by most cryonics advocates because this procedure destroys cellular viability and necessitates, as best as we can tell, advanced molecular nanotechnology or high magnification brain scanning as the only plausible means of revival. Another concern that has been raised is that freezing without cryoprotectant in the presence of a chemical fixative produces worse ultrastructural results than freezing alone. While modern vitrification technologies have somewhat removed this objection, this remains a serious concern for using the procedure post-mortem on ischemically compromised brains. In other words, if a brain completely vitrifies after chemical fixation it can produce superior results to normal vitrification but if it is just frozen, the fine structure may actually be worse off.
There is a subset of cases where both proponents and skeptics of ASC agree that the procedure might be the superior alternative. In cases where a patient is “stuck” at a funeral home due to regulatory or logistical challenges (the recent COVID-19 pandemic may be thought of as a potential example), perfusing the patient with a chemical fixative will still allow this patient to benefit from cryoprotection and avoid a straight freeze. A related scenario is one where a patient will be shipped to a cryonics organization, but the total transport time is such that cryoprotectant perfusion will occur in a severely ischemically compromised brain. We conducted several experiments to understand where this cut-off point may be and to understand the differences between several ASC scenarios. To our knowledge, these experiments constituted the first systematic investigation using ASC with CI’s VM-1 as the cryoprotectant, even before publication of the McIntyre paper.
Standard protocol in ASC (per McIntyre and Fahy’s 2015 Cryobiology paper) is to open the blood brain barrier (BBB) to prevent the extreme brain shrinking that is usually observed after cryoprotection with a vitrification solution. In our own research, we also recognized the importance of this protocol. Brains chemically fixed with glutaraldehyde and then cryoprotected with VM-1 without BBB modification show the same shrunken ultrastructure that is associated with conventional vitrification of the brain, a phenomenon that is increasingly being recognized as undesirable, despite the elimination of freezing. When the BBB was “opened” with the detergent Sodium Dodecylbenzene Sulfonate (SDBS), the ultrastructure of the brain looked normal and recognizable again.
One protocol change we were interested in was to see whether the chemical fixative could be omitted from the subsequent cryoprotection protocol after shipment of the patient. This would significantly simplify the protocol and would eliminate the need for the cryonics organization to add a chemical fixative to their vitrification solution (or change their carrier solution to make it compatible with the chemical fixative of choice.) When we limited the chemical fixation part only to the first step after blood washout, we obtained good results as well.
Is this procedure still feasible if there is a delay between the chemical fixation step and the cryoprotection step? To research this question, we delayed the cryoprotectant perfusion protocol by 48 hours (a conservative estimate of transport times from a funeral home to the cryonics organization). Cryoprotection was still possible and even produced whole-body weight loss, which is remarkable since substantial weight gain is usually observed after cryoprotection of ischemic patients. These results are very encouraging because it means the cryoprotection portion of ASC does not immediately have to follow the aldehyde-stabilization part of the procedure, allowing morticians to conduct this part without having to perform cryoprotectant perfusion.
Another possibility would be the ability of lesser trained mortuary personnel performing the aldehyde-stabilization portion of the procedure as near to clinical death as reasonably possible. This could be followed by a more highly trained individuals, a well trained local standby group, or a professional standby team being able to carry out field cryoprotection within the following 48 hour period. This would give several options for individuals for whom ASC might be appropriate and/or individuals for whom this is their method of choice in cryonics. It also gives some leeway in time for cases where the delayed arrival of advanced personnel is unavoidable and also would allow, under relatively normal circumstances, shipment to a cryonics service provider where the cryonics procedures could be continued.
What are the results of conducting ASC under sub-optimal ischemic conditions where chemical fixation is started after delays (hours or even days). We know from the vast literature on the “no-reflow” phenomenon, and research conducted in our lab, that after ischemic delays perfusion is compromised and ice formation is favored, despite the use of a vitrification solution. Similarly, compromised fixation after ischemic delays is routinely observed by histologists and experts in brain banking. In our own research we have found this to be the case as well. After 1 hour of normothermic ischemia or 24 hours of cold ischemia significant whole-body edema can be observed and ultrastructure is characterized by membrane damage, pale organelles, and visible red blood cells in the vessels (i.e. an indication of incomplete washout).
One potential solution to mitigate this problem is to delay the cryoprotection part to allow the chemical fixative the diffuse into poorly fixed tissue (a suggestion that had been proposed by some advocates of ASC). We did not, however, observe any positive effects on edema or ultrastructure from this approach. Chemical fixation is effective in stabilizing tissue, but it does not “seal” leaky vessels or restore compromised cell membranes. This protocol also has the potential risk of further worsening the fine structure of the brain because it permits further degradation of brain structure in poorly fixed areas of the brain.
Conclusion
All cryonics organizations often must respond to cases with no or little advance notification and, at times, in remote areas. This puts many patients at risk of post-mortem delays prior to starting cryopreservation procedures. One proposed solution is to deploy professional standby teams to the location of the patient. Not all members can afford such services and professional standby teams are not always able to deploy on time, even in cryonics patients for whom financing is not a problem.
We have reviewed and researched three major strategies for morticians to improve the outcome for a cryonics patient where professional standby is not possible: administration of medications, field washout and field cryoprotection, and aldehyde-stabilization. Timely administration of heparin and sodium citrate can improve cryoprotectant perfusion. Administration of an antibiotic can prevent bacterial overgrowth during transport.
Blood substitution by a mortician could also improve outcomes but requires pre-deployment of specific washout solutions and specific instructions for morticians to prevent over-pressurizing the patient and/or the introduction of air bubbles and particulates.
In principle, a mortician can do the surgery and procedures to do field cryoprotection but the logistical challenges of this procedure are even greater. Circulating highly concentrated and viscous cryoprotectants through a patient’s circulatory system goes far beyond a typical mortician’s familiarity level and comfort zone. In addition, field cryoprotection also requires the shipping or local fabrication of special insulated dry ice shipping box and compliance with dry ice shipping instructions. If field cryoprotection is attempted, it is best done with much forethought and preparation and the establishment of a useful training program for the local mortician and/or other personnel.
In principle, stabilizing a cryonics patient by perfusion of a chemical fixative is more in a mortician’s comfort zone as it more closely resembles embalming. Timely chemical fixation with formaldehyde or glutaraldehyde by a mortician, followed by cryoprotection at the cryonics facility can produce good preservation of the fine structure of the brain. Aldehyde-stabilized cryoprotection is no panacea, however, and delays affect chemical fixation to the same degree as they affect cryoprotection. Minimizing the delay between pronouncement of legal death and the start of procedures remains the biggest challenge for today’s cryonics organizations. The most effective solution to this challenge is not technical in nature but entails improving patient monitoring, incentives for relocation of terminal patients, and improving local response capabilities.
For the foreseeable future, morticians will play in important role in the logistical and legal aspects of cryonics. While there are ways in which properly trained and supervised morticians can assist in some kind of standby and preservation, this should not be an excuse for not for making credible arrangements with an SST provider. The procedures outlined in this article are explorations and should be not be read as a set of skills that most funeral directors can easily acquire.